Causes, Symptoms, Diagnosis & Treatment
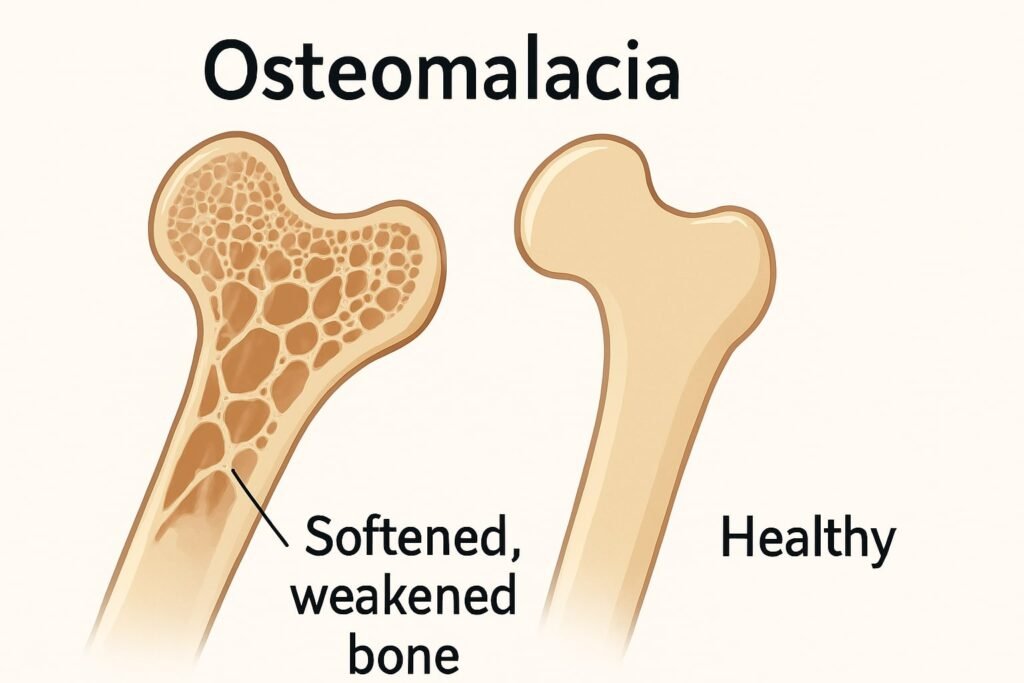
What Is Osteomalacia?
Osteomalacia is a bone-softening disorder. It stems from vitamin D deficiency and poor calcium absorption. Soft bones break easily. Adults get osteomalacia. Kids get rickets.
Osteomalacia Symptoms
- Bone pain in the hips, pelvis, and legs
- Muscle weakness and cramps
- Difficulty walking or altered gait
- Frequent falls and fractures
- “Pins-and-needles” in arms and legs
Causes & Risk Factors
- Low vitamin D from limited sun (“vitamin D deficiency”)
- Poor diet without fortified foods
- Malabsorption (celiac, Crohn’s)
- Bariatric surgery patients
- Darker skin pigment, covered clothing
- Age 65+, obesity, pregnancy
Diagnosis of Osteomalacia
- Medical history and physical exam
- Blood tests: low 25(OH)D, calcium, phosphorus; high ALP
- X-rays: look for Looser’s zones (pseudofractures)
- DEXA scan for bone density
- Bone biopsy if unclear
Osteomalacia Treatment
- High-dose vitamin D supplements
- Calcium and phosphorus boosters
- Sunlight exposure for natural D
- Weight-bearing exercises for bone strength
- Braces or surgery for severe deformities
- Monitor blood levels regularly
Prevention & Bone Health Tips
- Spend 10–30 minutes in the sun daily
- Eat fatty fish, fortified milk, and egg yolks
- Take vitamin D pills if needed
- Stay active with walking or lifting
- Screen high-risk groups early
Osteomalacia vs Osteoporosis
| Feature | Osteomalacia | Osteoporosis |
| Defect | Poor bone mineralization | Low bone mass, porous bones |
| Lab values | Low D, low Ca/P, high ALP | Normal Ca/P, normal ALP |
| Fracture pattern | Pseudofractures (Looser’s zones) | Vertebral, hip, wrist fractures |
| Bone density (DEXA) | Normal to low | Markedly low |
Further Comparison and Clinical Implications
While both osteomalacia and osteoporosis impair bone health, they differ fundamentally in their pathogenesis and management. In osteomalacia, defective mineralisation produces abnormally soft bones that can deform under normal loads, leading to characteristic pseudofractures (Looser’s zones). Lab studies reveal low vitamin D, calcium, and phosphorus, with elevated alkaline phosphatase—reflecting active but futile osteoid deposition. Treatment centres on replenishing vitamin D and minerals and correcting malabsorption, with rapid symptomatic relief once serum levels normalise.
Osteoporosis, by contrast, features an overall loss of bone mass and microarchitectural deterioration without a mineralisation defect. Serum calcium, phosphorus, and alkaline phosphatase typically remain within normal limits. Fracture prevention relies on antiresorptive or anabolic agents—such as bisphosphonates, selective estrogen receptor modulators, or teriparatide—alongside lifestyle measures to preserve existing bone and reduce fall risk.
Recognising these distinctions guides appropriate therapy: osteomalacia responds quickly to nutritional and sunlight interventions, whereas osteoporosis demands longer-term pharmacologic strategies to rebuild bone density and prevent fragility fractures.
Beyond the Basics: Related Insights
- Monitoring Trends: Global vitamin D insufficiency affects up to one billion people worldwide, highlighting the importance of routine screening in at-risk populations.
- Differential Diagnoses: Other causes of bone pain and low density—such as osteogenesis imperfecta, hypophosphatasia, and secondary hyperparathyroidism—should be ruled out with comprehensive biochemical panels.
- Emerging Diagnostics: Quantitative ultrasound and high-resolution peripheral quantitative computed tomography (HR-pQCT) are gaining traction for assessing bone quality beyond density alone.
- Patient Education Strategies: Visual aids, interactive apps, and community workshops can improve adherence to supplementation, dietary recommendations, and exercise regimens.
- Future Therapies: Novel agents targeting the Wnt signalling pathway and modulators of fibroblast growth factor 23 (FGF23) are under investigation and may offer new avenues for both disorders.